Researchers at the University of Amsterdam and affiliated institutions have developed a low-energy nebulization technique designed to deliver mRNA vaccines, such as those targeting SARS-CoV-2, via the respiratory tract. This approach aims to address degradation issues typically observed with conventional high-energy nebulization methods.
A Promising Alternative for mRNA Vaccine Administration
Inhalable vaccine delivery is particularly relevant for respiratory pathogens, as mucosal immunity in the airways may offer more immediate and localized protection. Most existing mRNA vaccines are administered via intramuscular injection, which is less effective in targeting mucosal surfaces. However, delivering mRNA vaccines directly to the lungs or nasal passages through aerosolized droplets presents technical challenges, primarily due to the sensitivity of lipid nanoparticles (LNPs) and mRNA molecules to mechanical stress.
The newly introduced nebulization method utilizes a nanotech membrane with significantly lower energy input, reducing mechanical degradation. This preserves both the LNP structures and the mRNA’s functional integrity, enabling the vaccine to remain biologically active post-nebulization.
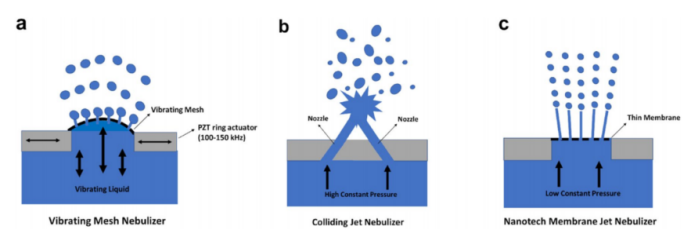
Figure 1. Methods for nebulization used in this study.
Addressing the Challenges of Aerosol-Based Delivery
High-energy nebulization methods, such as vibrating mesh (VM) and colliding jet (CJ), expose vaccine formulations to intense shear forces. These forces are known to disrupt LNPs and fragment mRNA, leading to reduced vaccine efficacy. The new method leverages a membrane with nanoscale pores, through which the vaccine is pushed at low pressure, minimizing energy dissipation to approximately 2 J/g—far below the 10–20 J/g threshold where mRNA degradation becomes significant.
Contributions and Key Findings
The study offers several contributions to the field of mRNA therapeutics, particularly regarding respiratory delivery:
Comparison Across Nebulization Methods:
Three nebulization systems were evaluated: vibrating mesh (VM1: ~35 J/g, VM2: ~18 J/g), colliding jet (CJ: ~22 J/g), and nanotech membrane (NM: ~2 J/g).
The nanotech membrane method consistently required the lowest energy input, significantly reducing the likelihood of LNP and mRNA damage.
Preservation of LNP Structure:
Dynamic light scattering (DLS) measurements showed that VM and CJ methods caused LNP aggregation and diameter shifts beyond 500 nm.
NM method preserved the original size distribution (300–500 nm), indicating minimal structural alteration to the nanoparticles.
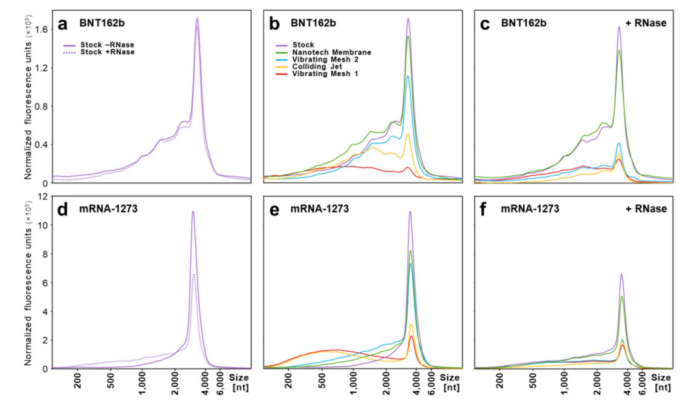
Figure 2: Effect of nebulization on mRNA integrity.
mRNA Integrity After Nebulization:
Gel electrophoresis revealed a 60–90% degradation in full-length mRNA using VM1 and CJ.
NM samples retained over 75–90% of full-length mRNA, both with and without RNase treatment, demonstrating that LNP encapsulation remained intact during the process.
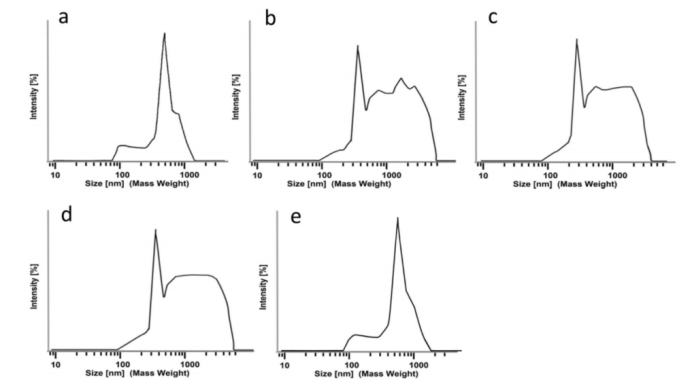
Figure 3: Particle size distributions of mRNA-1273 after nebulization.
Biological Functionality Maintained:
HEK293T cells exposed to NM-nebulized vaccines exhibited SARS-CoV-2 Spike protein expression levels similar to those treated with non-nebulized vaccines.
In contrast, VM and CJ methods led to a two- to fourfold reduction in Spike protein expression, confirming biological compromise due to degradation.
Energy Threshold Determination:
The study delineated clear energy dissipation thresholds: LNP rupture initiates above 5–10 J/g, while mRNA strand breakage occurs above 10–20 J/g.
The NM method’s energy input remains well below these thresholds, providing a safer window for respiratory vaccine administration.
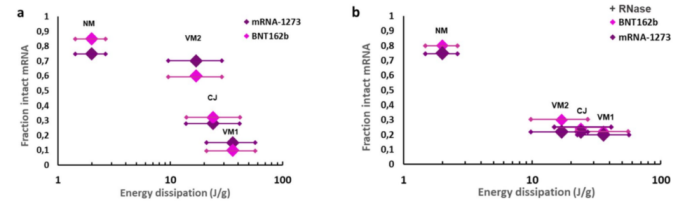
Figure 4: Fraction of intact mRNA versus nebulization energy dissipation.
Implications for Clinical Application:
The NM method can generate droplets predominantly in the 2–5 µm range, ideal for deposition in the alveolar and central airway regions.
Administration via NM nebulization could deliver standard vaccine volumes (0.05 mL) within 1–1.5 seconds, using devices such as a syringe-fitted nebulization chip.
Enhanced Suitability for Mucosal Delivery:
Given that RNases are abundant in respiratory mucosa, preserving LNP integrity is crucial for protecting mRNA payloads after delivery.
The low-energy method enhances the potential for effective mucosal immunity, a key advantage for respiratory-targeted immunization strategies.
Broader Implications for Vaccine Delivery
While the studied mRNA vaccines—BNT162b (Pfizer/BioNTech) and mRNA-1273 (Moderna)—were originally developed for intramuscular injection, the ability to maintain their integrity under low-energy nebulization suggests that future inhalable vaccines could benefit from this approach. Such delivery systems may be especially advantageous in regions with limited healthcare infrastructure, by simplifying administration and reducing the reliance on injections.
Additionally, this technique may be applicable to a broader range of RNA-based therapies aimed at treating respiratory illnesses beyond COVID-19, including influenza, tuberculosis, and emerging viral threats.
Conclusion
The development of a nanotech membrane-based low-energy nebulization method marks a significant step toward viable inhalable mRNA vaccines. By preserving both structural and functional components of mRNA-LNP formulations, this method addresses key limitations of high-energy nebulization systems. Future studies, particularly in vivo, will be essential to validate the long-term efficacy and safety of this approach, but the findings to date support its strong potential in expanding the landscape of vaccine delivery options.
Reference
van Rijn, Cees J. M., et al. “Low-Energy Nebulization Preserves Integrity of mRNA Vaccines for Respiratory Delivery.” Scientific Reports, vol. 13, no. 8851, 2023, https://doi.org/10.1038/s41598-023-35872-4.
