Editor: Sarah
A research team, led by Jiwei Sun and Tiantian Chen, has developed a bioadhesive hydrogel that shows promise in improving the healing of oral wounds in diabetic patients. This advancement comes in response to the specific challenges diabetes poses to wound healing, particularly in the oral cavity, where wounds are slow to heal due to factors like oxidative stress and immune dysfunction. The newly developed hydrogel, which mimics the adhesive properties of mussels, provides an effective solution for maintaining adhesion in the moist and dynamic oral environment. Furthermore, it combats oxidative stress, offering enhanced healing capabilities. This treatment represents a potential solution for diabetic patients suffering from chronic oral ulcers, which are known for their resistance to healing.
Challenges of Oral Wounds in Diabetic Patients
Diabetes poses significant challenges for the healing of oral wounds. The condition is often associated with delayed healing due to high glucose levels, increased oxidative stress, and immune system dysfunction. In the case of oral wounds, these factors lead to a pro-inflammatory environment that prolongs the healing process. Additionally, the constant presence of saliva and the dynamic oral environment further complicate the treatment of such wounds, making it difficult for traditional wound dressings to stay in place and be effective.
Limitations of Previous Treatments
Prior treatments, such as collagen dressings, growth factors, and other topical agents, have had limited success in treating oral wounds in diabetic patients. These options often fail due to high costs, poor adhesion in the moist environment of the mouth, or inability to address the underlying inflammation caused by oxidative stress. These limitations highlight the need for a more effective solution that can both adhere to mucosal surfaces and reduce inflammation.
A Dual-Function Bioadhesive Hydrogel
To address these challenges, the research team developed a bioadhesive hydrogel that combines both excellent adhesion properties and antioxidative effects. The hydrogel is inspired by the adhesion mechanism of mussels, which are able to strongly adhere to wet surfaces. This novel design allows the hydrogel to stay in place in the moist environment of the mouth, providing a continuous and stable treatment for oral wounds. Moreover, the hydrogel mimics natural antioxidative processes, which help to combat the oxidative stress that impedes healing in diabetic patients.
Positive Results in Animal Models
In animal trials using diabetic rats, the hydrogel demonstrated promising results. The rats treated with the hydrogel showed significantly faster wound healing and a reduction in inflammation compared to untreated wounds. These results suggest that the hydrogel could be an effective treatment for diabetic oral wounds, providing a practical solution to accelerate healing and reduce chronic discomfort in patients.
Potential for Broader Clinical Applications
While the hydrogel was initially developed to treat oral wounds, its potential extends beyond the oral cavity. The researchers believe that this hydrogel could be used to treat other types of chronic wounds, such as those in the gastric or liver regions, where similar challenges related to oxidative stress and immune dysfunction exist. The dual functionality of the hydrogel – both as an adhesive and an antioxidative agent – positions it as a versatile and innovative solution in the field of biomedical materials.
Contributions and Key Findings
- Innovative Bioadhesive Hydrogel Design: The researchers developed a mussel-inspired bioadhesive hydrogel, featuring a unique structure that ensures strong adhesion to mucosal tissues, even in the dynamic and wet environment of the oral cavity. The hydrogel is particularly designed to resist the washing effect of saliva and the physical disruptions caused by food and drink intake. Its ability to maintain adhesion during these challenging conditions offers a significant advantage over previous treatments for oral wounds.
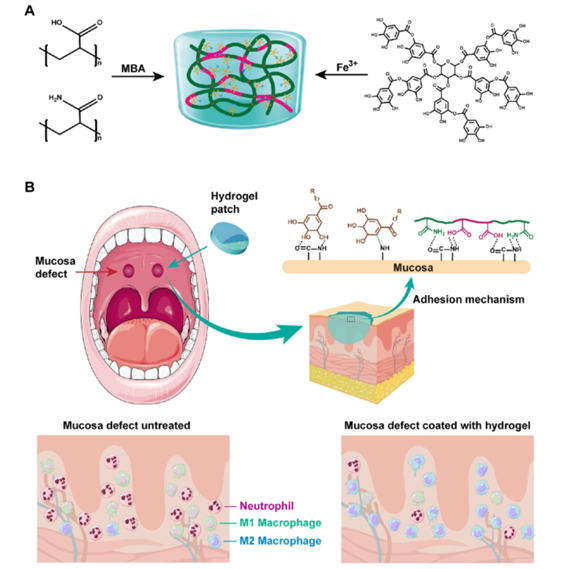
Figure 1: Formation and adhesion mechanism of an Fe-TA@P(AM-AA) hydrogel and its application.
- Effective in Reducing Oxidative Stress: A key feature of the hydrogel is its antioxidative capabilities. It mimics natural antioxidative processes, which are essential for mitigating the oxidative stress present in diabetic wounds. Diabetic patients often experience increased oxidative stress that impairs wound healing; thus, the hydrogel’s ability to scavenge harmful reactive oxygen species (ROS) promotes a healthier healing environment and reduces inflammation.
- Enhanced Wound Healing in Diabetic Models: Animal studies using diabetic rats demonstrated that the application of this hydrogel resulted in faster healing and reduced inflammation at the wound site compared to untreated controls. Specifically, the healing process was notably accelerated, with significant reduction in inflammatory markers, indicating that the hydrogel not only promotes tissue regeneration but also restores a more balanced immune response at the wound site.
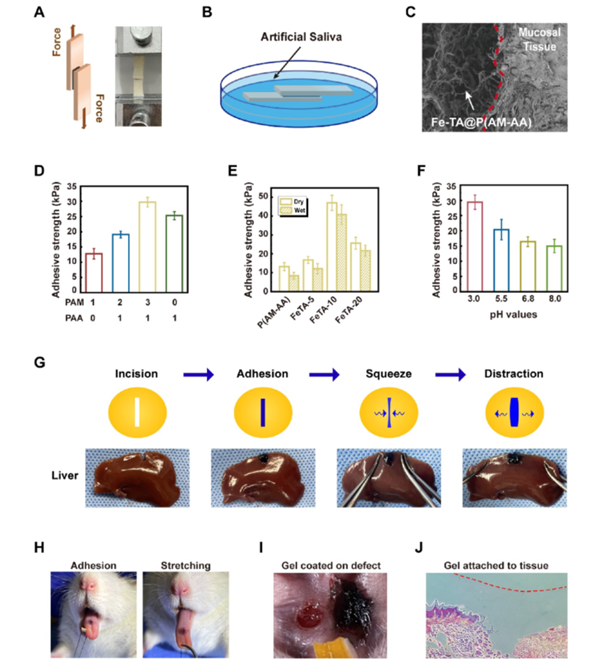
Figure 2: Adhesive performance of Fe-TA@P(AM-AA) hydrogel on rat oral mucosa.
- Mechanism of Action and Performance: The hydrogel’s adhesion is strengthened by a dynamic molecular interaction between its components and the tissue surface, particularly under acidic conditions that are often present in diabetic wounds. This adhesion mechanism, along with its antioxidative properties, makes the hydrogel particularly suited for use in diabetic patients who are prone to chronic inflammation and poor healing.
- Potential for Broader Clinical Applications: Although this hydrogel was developed specifically for oral wound healing in diabetic patients, its potential extends to other areas where chronic wounds and inflammation are concerns. This includes possible future applications in treating gastric ulcers, liver wounds, and other chronic injuries that are resistant to healing due to oxidative stress and immune dysfunction.
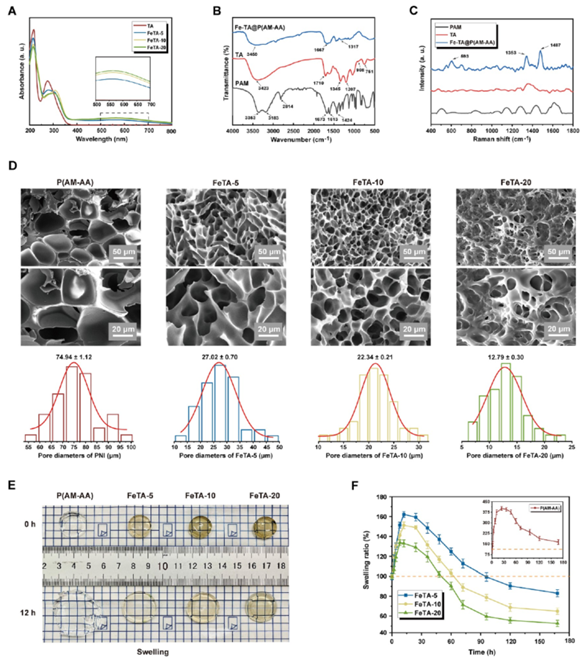
Figure 3: Swelling behavior and mechanical properties of Fe-TA@P(AM-AA) hydrogels.
- Superior Biocompatibility and Safety: The hydrogel has been tested for its biocompatibility, demonstrating no adverse effects on cell viability and showing no signs of cytotoxicity. This makes it a safe option for clinical use, minimizing the risks typically associated with some other wound-healing treatments.
Conclusion
In conclusion, this novel bioadhesive hydrogel offers a promising new therapeutic approach for treating chronic oral wounds in diabetic patients. By addressing both the mechanical challenges of wound care in a moist environment and the biological challenges posed by oxidative stress and inflammation, this hydrogel paves the way for more effective, practical treatments for chronic wounds.
Reference
Sun, Jiwei, et al. “Acceleration of Oral Wound Healing under Diabetes Mellitus Conditions Using Bioadhesive Hydrogel.” ACS Applied Materials & Interfaces, vol. 15, 2023, pp. 416-431. DOI: 10.1021/acsami.2c17424.
