Author: Tiffany
A recent study has shown that a novel hydrogel, which combines activated neutrophil-derived exosome mimetics with vascular endothelial growth factor (VEGF), significantly enhances the healing of chronic diabetic wounds while also providing antibacterial properties.
Key Highlights
- Research Question:
Can a hybrid hydrogel that combines activated neutrophil-derived exosome mimetics with VEGF enhance the treatment of chronic diabetic wounds? - Research Difficulties:
The challenges included low yields of neutrophil-derived exosomes and ensuring stable delivery of VEGF to the wound site. - Key Findings:
The developed VEGF-aPMNEM-ECM hybrid hydrogel not only promotes wound healing in chronic diabetic wounds but also shows effective antibacterial activity. - Innovative Aspects:
This study introduces a multifunctional hydrogel that utilizes exosome mimetics as carriers for VEGF, improving its stability and efficacy in a wound healing context. - Importance of the Study:
The research presents a promising therapeutic platform that could revolutionize the treatment of chronic diabetic wounds, potentially reducing the dependency on antibiotics.
Chronic Diabetic Wounds and Treatment Challenges
Chronic diabetic wounds are a significant and prevalent complication among individuals with diabetes, affecting approximately 19-34% of this population. The underlying pathophysiology of these wounds is complex, often resulting from a combination of factors, including chronic inflammation, impaired angiogenesis, and persistent microbial infections. These wounds typically exhibit symptoms such as prolonged healing times, swelling, and increased susceptibility to infection, which can lead to severe complications like ulcers and, in extreme cases, amputations. Traditional treatment modalities often involve antibiotics and growth factors, but these approaches face challenges, including drug resistance, reduced efficacy due to rapid degradation, and poor targeting of the wound site. As a result, there is an urgent need for innovative therapies that can effectively address the multifaceted nature of chronic diabetic wounds, combining antibacterial properties with strategies to promote healing and tissue regeneration.
Research Aim & Objectives
The research team, consisting of Yanzhen Yu, Hangfei Jin, Linbin Li, and others, conducted this study at the Affiliated Suzhou Hospital of Nanjing Medical University. The findings were published in the Journal of Nanobiotechnology in August 2023.
The primary aim of this research is to develop and evaluate a novel hybrid hydrogel that integrates activated neutrophil-derived exosome mimetics (aPMNEM) with vascular endothelial growth factor (VEGF) to enhance the treatment of chronic diabetic wounds. By combining these components, the study seeks to address the limitations of existing treatment modalities, particularly concerning the stability and efficacy of VEGF and the antibacterial properties of neutrophil-derived exosomes. Key objectives of the study include:
- Optimize the yield of activated neutrophil-derived exosome mimetics (aPMNEM) through an innovative extrusion process.
- Develop the VEGF–aPMNEM–ECM hybrid hydrogel for controlled release of VEGF and antibacterial properties.
- Conduct in vitro assessments of the hydrogel’s effects on endothelial cell migration, tube formation, and antibacterial activity.
- Evaluate the therapeutic effects of the hydrogel in a diabetic rat model, focusing on wound closure rates and tissue regeneration.
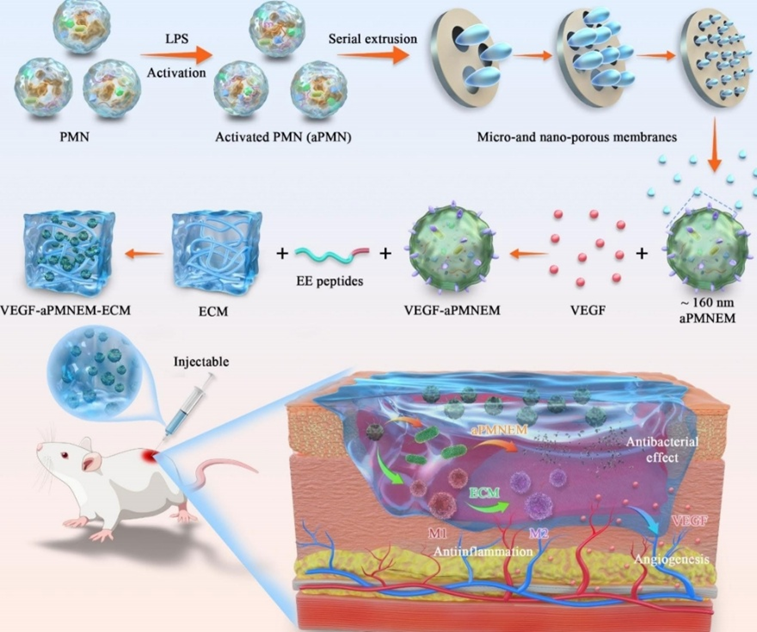
Figure 1. Scheme showing the study procedures.
Experimental Design and Key Findings
Experimental Process Outline
- Isolate polymorphonuclear neutrophils (PMNs) from human peripheral blood.
- Culture PMNs in RPMI 1640 medium supplemented with exosome-free fetal bovine serum.
- Activate PMNs using lipopolysaccharide (LPS).
- Prepare exosome mimetics (PMNEM) from PMNs through an extrusion process.
- Encapsulate vascular endothelial growth factor (VEGF) in activated neutrophil exosome mimetics (VEGF–aPMNEM) using ultrasound.
- Develop the VEGF–aPMNEM–ECM hybrid hydrogel.
- Conduct in vitro experiments to evaluate antibacterial activity, endothelial cell migration, and tube formation.
- Establish a chronic diabetic wound model in rats.
- Administer the VEGF–aPMNEM–ECM hydrogel treatment to diabetic wound models.
- Assess wound healing and perform histological analysis.
Key Experiments
1. Antibacterial Activity of aPMNEM
- Procedure: The in vitro antibacterial potential of aPMNEM against Escherichia coli and Staphylococcus aureus was assessed using the spread plate method. A suspension of 1.0 mL bacteria (107 CFU/mL) was incubated with 20 mL of aPMNEM (40 µg/mL) for 3 hours.
- Result: Following incubation, bacterial colonies were counted, showing significant inhibition of bacterial growth.
- New Finding: aPMNEM exhibited strong bacteriostatic effects, effectively reducing bacterial counts, indicating a potential alternative to antibiotics for treating infected chronic wounds.
2. Wound Healing in Diabetic Rat Model
- Procedure: A full-thickness skin wound model was created in diabetic rats, with a wound area of 2 cm diameter. The VEGF–aPMNEM–ECM hydrogel was administered at a dose of 500 µL. Wound areas were measured and photographed on days 1, 3, 5, 7, and 14 post-treatment.
- Result: The VEGF–aPMNEM–ECM treatment group exhibited a relative wound area reduction by day 14, compared to the PBS control group.
- New Finding: The VEGF–aPMNEM–ECM hybrid hydrogel significantly accelerated wound healing in diabetic rats, outperforming other treatment groups and demonstrating its potential for chronic wound management.
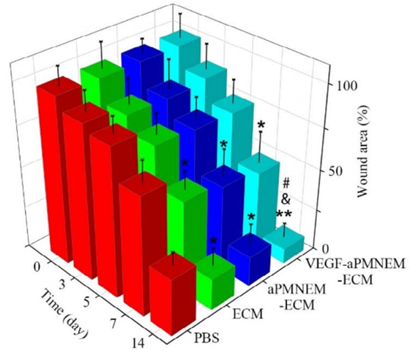
Figure 2. Quantitative analysis of relative wound area rates on days 1, 3, 5, 7, and 14.
3. Endothelial Cell Migration and Tube Formation
- Procedure: Human umbilical vein endothelial cells (HUVECs) were seeded and treated with PBS, ECM, aPMNEM–ECM, or VEGF–aPMNEM–ECM. Cell migration was evaluated using the scratch assay, while tube formation was assessed in Matrigel after 6 hours of treatment.
- Result: The VEGF–aPMNEM–ECM group showed the highest migration rate in the scratch assay, and significant tube formation was evident with increased total length and branching.
- New Finding: The VEGF–aPMNEM–ECM hydrogel effectively promotes endothelial cell migration and angiogenesis, crucial for wound healing, indicating its multifaceted role in tissue regeneration.
Implications and Future Improvements
This study presents a significant advancement in the treatment of chronic diabetic wounds through the development of a novel VEGF–aPMNEM–ECM hybrid hydrogel. The key findings demonstrate that this innovative hydrogel not only enhances wound healing rates but also possesses effective antibacterial properties. The incorporation of activated neutrophil-derived exosome mimetics (aPMNEM) with vascular endothelial growth factor (VEGF) improves the stability and efficacy of VEGF, while the extracellular matrix (ECM) provides a conducive environment for cell migration and tissue regeneration. These findings underscore the potential of this multifunctional hydrogel as a promising therapeutic platform, reducing reliance on traditional antibiotics and addressing the multifaceted challenges of chronic wound management.
Despite the encouraging results, the study acknowledges several areas for further improvement. The authors suggest exploring optimal administration methods and dosing intervals to maximize therapeutic effects. Additionally, quantifying the levels of VEGF in the exosome mimetics is essential to ensure consistent and effective delivery, enhancing the reliability of the treatment. Further research should also investigate the long-term effects and potential applications of the VEGF–aPMNEM–ECM hybrid hydrogel in other chronic conditions, thereby broadening its clinical relevance and therapeutic applications.
Reference:
Yu, Yanzhen, et al. “An injectable, activated neutrophil-derived exosome mimetics/extracellular matrix hybrid hydrogel with antibacterial activity and wound healing promotion effect for diabetic wound therapy.” Journal of Nanobiotechnology 21.1 (2023): 308.
